Overusing laboratory tests: more advantages or drawbacks?
After decades of accumulating evidence, the inappropriate use of laboratory services has now become a well-known critical issue. An interesting survey, just recently published in JAMA Internal Medicine (1), describes some interesting aspects concerning the prescription attitudes and the overuse of inpatient laboratory testing in a large American cancer center (i.e., Memorial Sloan Kettering Cancer Center, New York, NY, USA). Briefly, the percentage of physicians who agreed that hospitalized patients should have daily laboratory testing was close to 60%, whereas 55% of them were convinced that daily laboratory testing may be effective for increasing patient safety. These figures then translate in physicians disclosing that approximately 60% of laboratory testing was deemed to be actually unnecessary. This information is not really different from that reported in other studies, showing that the inappropriateness of laboratory testing can be as high as 70% (2).
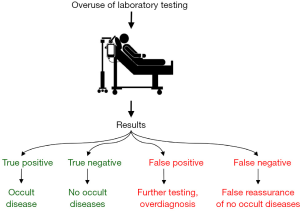
What clearly emerges from the interesting survey carried out at the Memorial Sloan Kettering Cancer Center, however, is that the vast majority of physicians were persuaded that non-clinically driven prescribing is not a questionable attitude, but also that routine testing, which is not apparently justified by the clinical context, may be somehow useful for increasing patient safety. The advantages and the inherent risks of inappropriate laboratory testing have been discussed many times before (Figure 1) (3), but can now be reaffirmed according to the results of the survey of Roman et al. (1). The main advantages are quite obvious, entailing reassurance that the patient has no “laboratory signs” of disease, especially when the negative predictive value of the test is close to 1.00 as for cardiac troponins measured with high-sensitivity immunoassays (4), or else enabling a possible diagnosis of an occult disease. A paradigmatic case is that of ordering hemoglobin testing in the elderly, wherein the clinical significance of large-scale screening studies in older subjects may contribute to make subclinical diagnosis of anemia, thus allowing a better and more effective therapeutic management, even if routine hemoglobin assessment is currently counterevidence (5). On the other hand, the putative drawbacks are not limited to the stemming waste of human and economic resources due to placing unnecessary orders to the laboratory, but also to the fact that inappropriate tests carry a high risk of producing false positive or false negative results, both of which can be causes of tangible risks, or even direct harm to the patients. In the unfortunate case that laboratory testing will produce a false negative result, this may then completely derange the clinical decision making by providing false reassurance that no occult pathologies are present. Thereby, the subsequent diagnosis of an occult disease already present at the time of test ordering may then be delayed, with possible detrimental impact on clinical outcomes. Unlike false negative test results, false positive test results (the probability of which is over 95% after the 19th laboratory test is ordered) (3), may then need follow-up investigations, to rule out the presence of occult diseases, so also placing unnecessary anxiety on both the physician and the patient. In the worst scenario, the physician may be driven to a wrong diagnosis or to the so-called “overdiagnosis” (e.g., in the case of prostate cancer screening by measuring prostate specific antigen) (6), thus generating detrimental effects on patient’s health due to inappropriate or unnecessary care.
Returning to the survey of the Memorial Sloan Kettering Cancer Center, it is then quite surprising that nearly 70% of physicians state that they would be comfortable if their hospitalized patients received less laboratory testing, a percentage increasing over 84% in attending and training physicians (1). This data seems actually conflicting with the prevalence of physicians who reported that inpatients should have daily laboratory testing (i.e., 60%). How can we explain such a difference? There is probably widespread perception that inappropriate test requesting is a real issue for health care, that this attitude is also somehow questionable, but physicians would be more comfortable if it is their colleagues who should perform less testing. This conviction is probably driven by perceived assurance that more tests may help preventing malpractice litigations, which are hence one of the most frequent causes of laboratory inappropriateness (7).
In conclusion, it is not so unlikely that the data of the Memorial Sloan Kettering Cancer Center actually reflects a widespread attitude concerning overuse of inpatient laboratory testing, thus further highlighting the need of developing universally agreed policies to overcome this concerning issue.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Journal of Laboratory and Precision Medicine. The article did not undergo external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jlpm.2017.06.15). Giuseppe Lippi serves as the unpaid Editor-in-Chief of Journal of Laboratory and Precision Medicine from November 2016 to October 2021. Martina Montagnana served as an unpaid Guest Editor of the series and serves as the unpaid Associate Editor-in-Chief of Journal of Laboratory and Precision Medicine from November 2016 to October 2021. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Roman BR, Yang A, Masciale J, et al. Association of Attitudes Regarding Overuse of Inpatient Laboratory Testing With Health Care Provider Type. JAMA Intern Med 2017; [Epub ahead of print]. [Crossref] [PubMed]
- Lippi G, Bovo C, Ciaccio M. Inappropriateness in laboratory medicine: an elephant in the room? Ann Transl Med 2017;5:82. [Crossref] [PubMed]
- Favaloro EJ, Lippi G. Reference ranges in hemostasis testing: necessary but imperfect. J Lab Precis Med 2017;2:18. [Crossref]
- Cervellin G, Mattiuzzi C, Bovo C, et al. Diagnostic algorithms for acute coronary syndrome-is one better than another? Ann Transl Med 2016;4:193. [Crossref] [PubMed]
- Pang WW, Schrier SL. Anemia in the elderly. Curr Opin Hematol 2012;19:133-40. [Crossref] [PubMed]
- Lee DJ, Mallin K, Graves AJ, et al. Recent changes in prostate cancer screening practices and prostate cancer epidemiology. J Urol 2017; [Epub ahead of print]. [Crossref] [PubMed]
- Montagnana M, Lippi G. The risks of defensive (emergency) medicine. The laboratory perspective. Emerg Care J 2016;12:17-9.
Cite this article as: Montagnana M, Lippi G. Overusing laboratory tests: more advantages or drawbacks? J Lab Precis Med 2017;2:41.