
Understanding cardiac troponin biology: all other cardiac biomarkers shall rest in peace?
The concept that high-sensitivity cardiac troponin immunoassays outperform creatine kinase MB (CK-MB) and myoglobin in the diagnostics of acute coronary syndrome has been put forward more than 10 years ago, and is now virtually incontestable. In the seminal study of Keller et al. (1), cardiac troponins, myoglobin and CK-MB were measured in over 1,800 consecutive patients admitted with suspected acute myocardial infarction. In all patients, the diagnostic performance (area under the curve, AUC) of both high-sensitivity cardiac troponin I (cTnI) (AUC, 0.96) and high-sensitivity cardiac troponin T (AUC, 0.85) was found to higher than that of both myoglobin (AUC, 0.82) and CK-MB (AUC, 0.73). Even more importantly, the early (i.e., <3 hours after onset of chest pain) negative and positive predictive values were also higher for high-sensitivity cTnI (0.94 and 0.82, respectively) than for myoglobin (0.87 and 0.64, respectively). The combination of highly-sensitive cardiac troponin immunoassays with either CK-MB or myoglobin did not improve the diagnostic performance of highly-sensitive cardiac troponin immunoassays alone, thus making the assessment of other biomarkers virtually meaningless. These results were then confirmed by many ensuing studies, such as that of Kitamura et al. (2), who showed that the combination of the early negative (1.00 vs. 0.37) and positive (0.93 vs. 0.93) predictive values of high-sensitivity cardiac troponin immunoassays offset those of CK-MB.
Although many international guidelines and recommendations have now thoughtfully endorsed the measurement of cardiac troponins as the one and only biochemical strategy for ruling out or diagnosing myocardial injury, thus including acute myocardial infarction (3), several lines of evidence attest that some other traditional biomarkers are still prescribed alongside cardiac troponins by many physicians. Overall, the worldwide combined measurement of cardiac troponins with CK-MB and/or myoglobin has been reported to be as high as 30%, with notable exceptions, even approximating 50% (4,5). The reasons beyond this attitude are many and multifaceted, and basically include a well-known resistance to change, disinformation, poor knowledge of diagnostic performance of cardiac biomarkers, along with personal persuasions that CK-MB and/or myoglobin would provide more useful clinical information than cardiac troponins. Beside these well-known drawbacks, another false myth that surrounds cardiac troponins, is that they would display a delayed kinetics compared to both CK-MB and/or myoglobin.
Studies on patients with different forms of acute myocardial injury shall not be thoughtfully regarded as the gold standard for mirroring troponin kinetics. This is actually due to the fact that the correspondence between cardiac damage and its signs and symptoms is not unequivocal and straightforward, whereby many patients cannot exactly refer (or remember) the time of symptoms onset. More reliable information might hence be garnered from exercise physiology (6), since the time between cardiac stress and biomarker release can be more accurately defined (7). Valuable information on this aspect has been generated by the ongoing research project called “Run for Science”, which encompasses studying the release of many conventional and innovative biomarkers after different forms of endurance exercise (8). In the half-marathon subset of this study, which is indeed a less demanding form of recreational activity than running a marathon or an ultra-marathon, the early kinetics of a huge number of cardiac biomarkers has been investigated, thus including cardiac troponins, myoglobin and CK-MB. The most interesting findings are shown in Figure 1. Quite interestingly, immediately after the end of the 21 km run (lasting approximately 90 min), the values of cTnI measured with a high-sensitivity immunoassay were nearly double than those at the baseline, further increasing with a virtually perfect linear fit toward ~4- and ~5-fold higher concentration 3 and 6 hours afterwards. Nearly overlapping data were published by Liebetrau et al. in patients undergoing transcoronary ablation of septal hypertrophy (9). Values exceeding the method-specific diagnostic threshold were recorded as soon as 15 min after the intervention for cardiac troponins measured with a high-sensitivity immunoassay, after 30 min for myoglobin, whilst a diagnostic concentration of CK-MB could only be observed after 90 min.
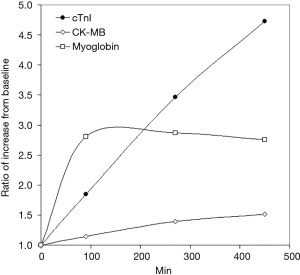
Comparing these data with those of other biomarkers (10), it seems rather clear that the kinetics of CK-MB is definitely less efficient than that of cTnI for early detecting cardiac sufferance, as shown in Figure 1. Not only the kinetics appears slower, but also the relative increase is considerably lower than that of cTnI. The early kinetics of myoglobin also exhibits a different trend, whereby the sharp, sudden increase is then counterbalance by a curve flattening, which would actually challenge the identification of a continuous rise (or fall) of biomarker values, as mandated by current guidelines (1) (Figure 1).
This reliable evidence shall hence reassure even the more sceptic clinicians that the measurement of cardiac troponins with high-sensitivity immunoassays would provide more “biologically” sensible information than the assessment of either CK-MB or myoglobin. The combined measurements of two or more cardiac biomarkers not only appear biologically unwarranted (11), but may also carry additional biological, clinical, analytical and economic drawbacks, as summarized in Table 1 (12,13). Although part of the biological background has been discussed before, it is also worthwhile mentioning here that—unlike cardiac troponins—both CK-MB and myoglobin are not cardiospecific, since these proteins are contained at variable extent in many other muscular districts (7). Even if the term “high-sensitivity” has been originally coined for emphasizing the improved analytical (and not diagnostic) sensitivity, several reliable evidences have then been published that the diagnostic performance of CK-MB and myoglobin is consistently lower than that of cardiac troponins, especially when these last biomarkers are assayed with highly-sensitive techniques. Neither their combined measurement seems to further increase the clinical efficiency of measuring cardiac troponins alone. It shall also not be discounted the fact that maintaining CK-MB and myoglobin within panels for diagnosing myocardial injury would encumber clinicians from accurately understanding how cardiac troponins should be appropriately and effectively used in clinical practice. Notably, recent evidence has also been provided that cardiac troponin values are not only useful for diagnosing myocardial injury, but also for short and long-term prognostication (14), whilst no similar information can be garnered from measuring CK-MB or myoglobin. According to an economical perspective, CK-MB and myoglobin do not seemingly provide useful (incremental) information to the clinical decision making, whilst their cost is globally comparable to that of cardiac troponins in most healthcare facilities. Performing additional tests would have an impact on the organization of laboratory services, which are already facing a hard time for managing increased volumes and complexity (15). This would lead us to conclude that measuring CK-MB, myoglobin or both shall be considered no longer cost-effective. As a final consideration, it should be noted that quality assessment of CK-MB and myoglobin is at least as difficult as, if not more challenging than, that of cardiac troponins. For example, the lower the number of laboratories which would still measure CK-MB, the less likely the chance that the results of external quality assessment (QEA) schemes would provide reliable performance information to the laboratory.
Table 1
| Biological |
| CK-MB and myoglobin are not cardiospecific |
| Kinetics is less informative than that of cardiac troponins |
| Clinical |
| Lower diagnostic performance, alone or in combination with cardiac troponins |
| Lower understanding on how cardiac troponins should be used in clinical practice |
| Lack of prognostic clinical information |
| Economic |
| CK-MB and myoglobin are as expensive as high-sensitivity cardiac troponin immunoassays |
| Overcrowding of test menus |
| Analytical |
| Challenging quality assessment (e.g., external quality assessment) |
Although the global diagnostic market of cardiac biomarkers remains heterogeneous, many convincing evidences were brought that there is no reliable alternative to measuring cardiac troponins alone (16). Even firm detractors of this assumption shall now be persuaded that CK-MB and myoglobin must rest in peace for the diagnostics of acute cardiac injury.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was a standard submission to the journal. The article was sent for external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jlpm.2019.02.03). Giuseppe Lippi serves as the unpaid Editor-in-Chief of Journal of Laboratory and Precision Medicine from November 2016 to October 2021. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Keller T, Zeller T, Peetz D, et al. Sensitive troponin I assay in early diagnosis of acute myocardial infarction. N Engl J Med 2009;361:868-77. [Crossref] [PubMed]
- Kitamura M, Hata N, Takayama T, et al. High-sensitivity cardiac troponin T for earlier diagnosis of acute myocardial infarction in patients with initially negative troponin T test--comparison between cardiac markers. J Cardiol 2013;62:336-42. [Crossref] [PubMed]
- Cervellin G, Mattiuzzi C, Bovo C, et al. Diagnostic algorithms for acute coronary syndrome-is one better than another? Ann Transl Med 2016;4:193. [Crossref] [PubMed]
- Galli GA, Malloggi L, Moretti M, et al. The IV survey of GdS MM SIPMeL: state of the art of “necrosis” cardiac markers in Italy. Riv Ital Med Lab 2018;14:87-96. [Crossref]
- Lippi G, Mattiuzzi C, Cervellin G. Trends of popularity of cardiac biomarkers: Insights from Google Trends. Emerg Care J 2018;14:7769. [Crossref]
- Lippi G, Schena F, Dipalo M, et al. Troponin I measured with a high sensitivity immunoassay is significantly increased after a half marathon run. Scand J Clin Lab Invest 2012;72:467-70. [Crossref] [PubMed]
- Lippi G, Schena F, Ceriotti F. Diagnostic biomarkers of muscle injury and exertional rhabdomyolysis. Clin Chem Lab Med 2018;57:175-82. [Crossref] [PubMed]
- Lippi G, Schena F. Run for Science (R4S): the history of a successful project of precision and laboratory medicine in sport and exercise. J Lab Precis Med 2017;2:11. [Crossref]
- Liebetrau C, Möllmann H, Nef H, et al. Release kinetics of cardiac biomarkers in patients undergoing transcoronary ablation of septal hypertrophy. Clin Chem 2012;58:1049-54. [Crossref] [PubMed]
- Lippi G, Schena F, Salvagno GL, et al. Acute variation of biochemical markers of muscle damage following a 21-km, half-marathon run. Scand J Clin Lab Invest 2008;68:667-72. [Crossref] [PubMed]
- Mair J, Lindahl B, Hammarsten O, et al. How is cardiac troponin released from injured myocardium? Eur Heart J Acute Cardiovasc Care 2018;7:553-60. [Crossref] [PubMed]
- Saenger AK, Jaffe AS. Requiem for a heavyweight: the demise of creatine kinase-MB. Circulation 2008;118:2200-6. [Crossref] [PubMed]
- Alvin MD, Jaffe AS, Ziegelstein RC, et al. Eliminating creatine kinase-myocardial band testing in suspected acute coronary syndrome: a value-based quality improvement. JAMA Intern Med 2017;177:1508-12. [Crossref] [PubMed]
- Plebani M, Antonelli G, Zaninotto M. Cardiac biomarkers of acute coronary syndrome: from history to high-sensitive cardiac troponin. Intern Emerg Med 2017;12:143-45. [Crossref] [PubMed]
- Plebani M, Laposata M, Lippi G. A manifesto for the future of laboratory medicine professionals. Clin Chim Acta 2019;489:49-52. [Crossref] [PubMed]
- Giuliani S, Dieplinger B, Mueller T. Head-to-head comparison of three different high-sensitivity cardiac troponin assays for early rule-in and rule-out of acute myocardial infarction. J Lab Precis Med 2019;4:4. [Crossref]
Cite this article as: Lippi G, Plebani M. Understanding cardiac troponin biology: all other cardiac biomarkers shall rest in peace? J Lab Precis Med 2019;4:9.


