
Point-of-care high-sensitivity troponin assays: advancements, clinical applications, and implementation considerations
Introduction
For many years cardiac biomarkers have played a pivotal role in the diagnosis of acute myocardial infarction (AMI) and in the diagnostic pathways for patients presenting to hospitals with suspected AMI. Immunoassays for cardiac troponins (cTn) were developed in the late 1980s (1,2) and greatly enhanced the diagnostic accuracy of the biochemical diagnosis of AMI. Previously used biomarkers such as lactate dehydrogenase, aspartate aminotransferase, myoglobin, creatine kinase (CK), and its myocardial band isoenzyme (CK-MB) all lacked specificity for myocardial tissue, making them difficult to interpret and use in clinical practice. cTnI and cTnT are exclusively released from cardiomyocytes. Measurements therefore have a high specificity for myocardial tissue injury and a corresponding high clinical sensitivity for AMI. Measurements of cTn soon became the biochemical gold standard in diagnosing AMI and has been included in the Universal Definition of Myocardial Infarction (UDMI) for decades (3-6). The UDMI bases the diagnosis of AMI on clinical evidence of myocardial ischemia along with a detection of a rise and/or fall of cTn with at least one value above the 99th upper reference limit. Since the 4th UDMI was released in 2018 troponins are also being used to define acute and chronic myocardial injury, including non-ischemic causes of cardiac injury (3).
Troponin assays have progressively improved and since 2009, high-sensitivity cardiac troponin (hs-cTn) assays have been available. To be defined as high-sensitive, a troponin assay should have an analytical variation (CVA) of less than 10% at the concentration corresponding to the 99th percentile for that assay, determined in a cohort of healthy individuals. Furthermore, troponins should be measurable [above the limit of detection (LoD) for the assay] in more than 50% of healthy individuals, stratified by gender (50% of women and 50% of men) (7). The adherence to this recommendation is not complete, as some manufacturers might claim high-sensitivity even though struggling to provide quantitative results in more than 50% of healthy subjects. This requirement is especially challenging in women and/or after rigorously screening for subclinical disease (8).
Implementation of hs-cTn measurements have led to enhanced diagnostic accuracy of AMI at an early stage after onset of symptoms (9,10). Significant increases above the LoD of the assay are usually detectable within 2–3 hours and delta values between two measurements within 1 hour (11). Algorithms measuring baseline and 1–2-hour troponin deltas have a high accuracy for identifying individuals with high or low risk of subsequently developing non-ST elevation myocardial infarction (NSTEMI) in patients with symptoms suggestive of myocardial infarction (11-19), and are recommended by international societies including the European Society of Cardiology (ESC) (20).
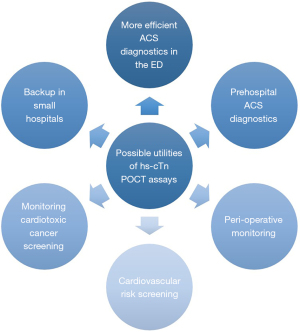
Measurements of hs-cTn are furthermore recommended for risk prediction in patients undergoing non-cardiac surgery (21) and cardiotoxic cancer therapy (22). The known ability to predict long-term cardiovascular risk (23-27) is currently not translated into clinical practice as there is no consensus in how to use troponin measurements to modify cardiovascular risk.
Traditionally, troponin analyses have been performed by central laboratory testing (CLT) and by point-of-care testing (POCT), depending on practicalities. This balance shifted towards CLT when high-sensitivity troponin assays were launched, as no hs-cTn POCT assays were available. In the past few years, cTn POCT assays achieving high-sensitivity criteria have been developed (7,28). The current paper discusses the potential utility of POCT hs-cTn assays and outline some important prerequisite necessary before hs-cTn assays may be implemented, both practically and scientifically.
What kind of hs-cTn POCT assays do we have today?
Compared to CLT, a POCT instrument should be compact enough to be used at or near the site of patient care. It should also be user-friendly, possible to operate by non-laboratory personnel and utilise whole blood samples to avoid the need of sample preparation such as centrifugation and pipetting steps. Technically a conventional instrument used in an area proximate to the patient could be defined as a point-of-care assay. However, this is not the common interpretation and in this article, we will only discuss desktop or portable instruments.
According to the tables provided on the website from the International Federation of Clinical Chemistry Committee of Clinical Application of Cardiac Bio-Markers (IFCC C-CB) (29) there are three POCT instruments currently fulfilling the criteria for a hs-cTn assay; the PATHFAST (LSI Medicine Corporation, Tokyo, Japan), the TriageTrue (QuidelOrtho, San Diego, United States) and the Atellica VTLi (Siemens Healthineers, Erlangen, Germany). It should be noted that the availability of these instruments may vary around the world depending on local regulatory approval. These assays have been validated for use in whole blood and plasma. The key analytical characteristics of the assays are presented in Table 1, which has been adapted from the IFCC C-CB webpage. The IFCC tables include information as provided by the manufacturer and are regularly updated.
Table 1
| Platform | Assay | Company | %CV at 99th percentile | LoB (ng/L) | LoD (ng/L) | 99th percentile (ng/L) | Percent normal measured > LoD |
|---|---|---|---|---|---|---|---|
| PATHFAST | hs-TnI | LSI Medicine Corporation (formerly Mitsubishi) | 6.1* | 1.23 | 2.9 | Overall: 27.9; F: 20.3; M: 29.7 | Overall: 66.3; F: 52.8; M: 78.8 |
| TriageTrue | hs-TnI | QuidelOrtho | 5.0–5.9 at 21 ng/L (plasma); 5.9–6.5 at 22 ng/L (WB)* | 0.4 (plasma); 0.5–0.8 (WB) | 0.7–1.6 (plasma); 1.5–1.9 (WB) | Overall: 20.5; F: 14.4; M: 25.7 | Overall: ≥50 |
| Atellica VTLi | hs-TnI | Siemens Healthineers | 6.5 (plasma); 6.1 (WB)* | 0.55 | 1.2 (plasma); 1.6 (WB) | Overall: 22.9; F: 18.5; M: 27.1 | Overall: 84; F: 80; M: 87 |
*, the analytical CV (%) at the 99th percentile was obtained under optimized laboratory conditions. As POCT devices are generally used by multiple operators, the imprecisions will be expected to be higher on a routine basis. POCT, point-of-care testing; CV, analytical coefficient of variation; LoB, limit of blank; LoD, limit of detection; hs-cTn, high-sensitivity cardiac troponin; F, female; M, male; WB, whole blood.
PATHFAST is a benchtop immunoassay analyzer that can analyse up to 6 parameters simultaneous including hs-cTnI, myoglobin, CK-MB, D-dimer, N-terminal pro-B-type natriuretic peptide (NT-proBNP) and high-sensitivity C-reactive protein (hsCRP) and provides results within 17 min. Although the PATHFAST uses single test cartridges and no additional buffers are required, it is larger and does require a higher degree of operator skill than the other available POCT assays. The TriageTrue is an immunoassay analysed on the QuidelOrtho Triage MeterPro device providing high-sensitivity troponin I (hs-TnI) results in <20 min. It is portable and can run approximately 100 tests on batteries. The MeterPro can also run other assays such as NT-proBNP, D-dimer and a urine tox drug screen. Finally, there is the Atellica VTLi, which is a portable immunoassay analyser with battery capacity for up to 60 tests providing hs-TnI in 8 min. In addition to whole blood and plasma the VTLi has also been validated for use in capillary blood. There are currently no other assays available on the device. Additionally, there are several other hs-cTn POCT systems currently undergoing development.
Barriers to implementing accelerated diagnostic protocols for investigating acute chest pain
Overcrowding in the emergency department (ED) has been shown to increase mortality, costs and length of stay (30,31). Accordingly, there is a need for more efficient management of patients with symptoms suggestive of acute coronary syndrome (ACS). Such patients contribute to a substantial proportion of admissions, even though less than 25% are eventually diagnosed with ACS (9,10). In some regions ACS rates might be even lower, due to variation in use of ED and prehospital services (32,33). Different protocols have been suggested in order to accelerate triage, reduce time to diagnosis and thereby decrease dangerous overcrowding in the ED and reduce cost. Accelerated diagnostic protocols usually combine a troponin algorithm with clinical judgement (20), typically standardized as a clinical risk score (34). The most commonly used troponin algorithms are those of the ESC (20) and the high-STEAC (The High-Sensitivity Troponin in the Evaluation of patients with suspected Acute Coronary Syndrome-study) investigators (13).
These algorithms have proven slow and difficult to implement, as found in a survey reporting current practice in European and American laboratories (35). Clinically, trust and adherence to the algorithms have been suboptimal as demonstrated in the High-US study where 42.7% of 1,020 patients were admitted in spite of meeting ESC 0/1-hour rule-out criteria for ACS (36). Obstacles to the implementation of the accelerated diagnostic protocols reflect logistic and practical issues within the institution. An important component in this complex puzzle is the actual turnaround time (TAT) (defined as time from blood sampling to reporting the result) for analyzing cTns. Traditionally a maximum TAT of 60 min has been recommended (5). Although central laboratory platforms may use STAT (STAT is an abbreviation of statim that means “immediately”) assays, delays due to sample transport, centrifugation or reporting of results may lead to TAT exceeding 60 min (37). Some protocols suggests that AMI rule-out can be achieved based on a single sample at baseline (if the time from onset of symptoms exceeds 3 hours) (20). If the CLT cannot produce a result for the admission sample within 1 hour, a decision cannot be made until after the 1-hour draw, obviating the possibility of rule-out at presentation. Currently, the ESC algorithm suggests that a 1-hour sample may be feasible in all patients, if the TAT is ≥60 min (20). Accordingly, the patients may need to stay in the ED for up to 2–3 hours until a final risk prediction regarding NSTEMI can be made. Incorporation of hs-cTn POCT assay with substantially shorter TAT could therefore potentially reduce time in the ED, leading to a significant improvement in patient care.
Benefits and future use of POCT
Efficiency benefits in the ED
POCT has the ability to provide a swift result directly to the clinician. The overall time-saving should lead to shorter time to diagnosis, shorter time to treatment and more rapid discharge or disposition decisions. However, previous studies utilizing different strategies incorporating POCT in ACS diagnostics have shown divergent impacts on time and cost efficiency (38-42). These studies documented that the presence of a structured decision-making protocol was a crucial prerequisite for efficient utilizing the POCT cTn measurements. High-sensitivity troponin assays or current 0/1-hour algorithms were not tested. The ability for rapid rule-out would be expected to be higher when hs-POCT assay are utilized in accelerated diagnostic protocols including dedicated and assay specific rule-out algorithms. Reports from the derivation and validation of assay- specific cut-offs for accelerated protocols for the new hs-POCT assays have shown similar rule-out capability to measurements by central laboratory assays (32,43,44). To date there are validated assay specific cut-offs for the 0/1-hour algorithm and for single sample rule-out for the PATHFAST and TriageTrue assays (43,44), whilst cut-offs for a single sample rule-out have been published for the Atellica VTLi (32) (Table 2). It should be noted that the first published algorithm cut-offs for PATHFAST and TriageTrue were derived using biobanked samples and analyzed in a laboratory setting (43,44), questioning the validity and applicability when using whole blood in an ED setting. In the recent publication that suggested a single sample cut-off for the Atellica VTLi, this was derived from fresh whole-blood [Safe Emergency department dIscharGE (SEIGE) study] and subsequently validated in frozen plasma samples [Suspected Acute Myocardial Infarction in Emergency (SAMIE) study] (32).
Table 2
| Platform | Practical features | Validated cut-offs | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Size (cm) | Time to results (min) | Specimen type | Instrument type | Single sample rule-out (ng/L) | NPV (95% CI) (%) | ESC 0/1 rule-out (ng/L) | NPV (95% CI) (%) | ESC 0/1 rule-in (ng/L) | PPV (95% CI) (%) | ||
| PATHFAST | 34.0×57.0×48.0 | 17 | WB/plasma | Benchtop | <3* | 98.1 (96.1–99.4) | <4 and delta <3 | 100.0 (97.7–100.0) | ≥90 or delta ≥20 | 86.5 (77.6–92.8) | |
| 99.7 (98.1–100.0) | |||||||||||
| TriageTrue | 21.6×15.8×6.4 | <20 | WB/plasma | Portable | <4* | 100.0 (99.4–100.0) | <5 and delta <3 | 100.0 (98.8–100.0) | ≥60 or delta ≥8 | 76.8 (67.2–84.7) | |
| Atellica VTLi | 25.0×8.5×5.0 | 8 | WB/plasma/capillary | Portable | <4* | 99.5 (97.2–100.0) | TBD | – | TBD | – | |
Cut-offs apply irrespective of age and renal function. *, requires >3 h from symptom onset. POCT, point-of-care testing; CI, confidence interval; NPV, negative predictive value for acute coronary syndrome; PPV, positive predictive value for acute coronary syndrome; ESC, European Society of Cardiology; WB, whole blood; TBD, to be determined.
When using rapid rule-out strategies for ACS, it should be borne in mind that chest pain patients might need other investigations such as D-dimer or a chest X-ray to exclude other diagnosis. These investigations might require longer waiting times, diminishing the potential ED-efficiency gain of POCT. Accordingly, hs-cTn POCT assays can only be expected to improve logistics for patients where troponin results are the time-limiting step for the flow through the ED. However, the use of POCT may allow for faster diagnoses in critically ill patients by aiding in differentiation between cardiac diseases such as AMI and life threatening non-cardiac disorders such as aortic dissection or Boeerhaves syndrome, providing an important tool in the armamentarium of emergency physicians.
Increased availability
Increased availability is another potential change brought about by the introduction of hs-cTn POCT assays that might benefit patient care (Figure 1). Since the devices are small and can be operated by non-laboratory personnel they could be used whenever there is a need for a troponin test including circumstances without access to a central laboratory or laboratory staff or where such access is limited. There are several situations where this could be applicable both outside and within larger health care institutions.
Utility of hs-cTn in a prehospital setting
Primary care functions as a gatekeeper to more specialized health care systems. As there has been a lack of decision aids to safely rule-out ACS in primary care (45) most patients go to the ED for investigations (either directly or after referral from primary care physicians) when symptoms of possible ACS occur (46,47). Contemporary POCT instruments have been infrequently used in outpatient clinics and ambulances. The low diagnostic sensitivity requires use of prolonged observation and serial measurement (>6 hours) for investigating possible NSTEMI. After hs-cTn came into routine use in central laboratories the benefit of contemporary POCT assays diminished. Even so, it is still our experience that contemporary cTn POCT assays have been used in rural areas with difficult access to advanced health care facilities, particularly in patients perceived as low risk for ACS and where transport is not straightforward or timely. Strategies to improve prehospital triage and safe reduction in referrals of chest pain patients to the ED have also been studied. Newly published data from the FamouS Triage study showed that a prehospital HEART (History, Electrocardiogram, Age, Risk Factors, and Troponin) score combined with contemporary POCT cTnT measurements in the ambulance could avoid hospital admission of low-risk patients (48). This strategy showed non-inferiority for safety compared to routine care. A recent retrospective study from Norway demonstrated acceptable safety and better cost-effectiveness when applying the 0/1-hour hs-cTnT ESC algorithm in an outpatient clinic staffed by primary care physicians (49,50). Cost-effectiveness in low-risk patients was compared between an algorithm utilizing 0/1-hour hs-cTnT samples that were taken in outpatient clinics and transported to the local hospital for analyses and standard patient care that required admission to a general hospital that measured hs-cTnI at admission and approximately 6 hours later. The study suggested that prehospital measurements would allocate patients to the right level of health care earlier, shortening their time of contact to the health care, and restrict the needs for transport to a lower number of patients. Another recent and promising report from the URGENT 1.5 study using a modified HEART score with a capillary POCT hs-cTnI in a prehospital setting showed similar risk stratification ability compared to standard HEART score with venous CLT hs-cTn results (51). However, further validation is needed as this study was small and the data collection was done retrospectively. Thorough studies confirming the utility and efficiency of hs-cTn POCT outside of hospitals are therefore warranted.
Another out of hospital situation where hs-cTn POCT could be beneficial are institutions such as nursing homes or other facilities providing long-term health care for selected patient groups. In such institutions troponin measurements could be used as part of a panel of tests improving diagnostic accuracy and prioritizing appropriate further treatment. This could prevent uncomfortable and possibly dangerous transfer of patients with severe comorbidities. Depending on the competence within the institution local treatment of AMI could be preferred in patients with severe cognitive impairment, as transportation might trigger anxiety or delirium leading to severe deterioration of the underling condition and a poorer prognosis.
In sum, there seems to be a large potential for future out of hospital troponin-based algorithms that could reduce unnecessary patient influx to the ED or allocate patients directly to the cardiac ward even before presenting to the hospital.
Clinical utility of hs-cTn in other conditions than ACS
As the evidence base increases, troponin measurements are expected to be used in several clinical settings not directly related to ACS. Measurements of cTns are recommended in the pre and postoperative setting (21). The updated ESC guideline for cardiovascular assessment and management in non-cardiac surgery suggest that perioperative troponin changes are estimated in patients undergoing intermediate or high-risk surgery. The delta values are used to diagnose perioperative myocardial injury (PMI), a condition signalling increased long-term risk of mortality and morbidity (21). The institutions performing these procedures will usually have access to CLT, but if that is not the case such as in specialized orthopaedic or surgery-only hospitals, using a POCT hs-cTn assay could be a cost-effective and safe alternative.
Second, troponin and natriuretic peptide measurements are also suggested for risk assessment before and monitoring during cardiotoxic cancer treatment (22). Cancer patients may have increased cardiovascular risk due to the treatment provided or due to the malignant disease itself and pre-treatment cardiac biomarker screening is recommended for large groups of patients (22). Some malignant diseases also need cardiac biomarker monitoring between treatment cycles, for instance breast cancer treated with anthracyclines or human epidermal growth factor receptor 2 (HER2)-targeted treatments (22). If the oncology centre has limited access to central laboratory facilities or the service provided is too slow to accommodate treatment-adjustments during outpatient consultation (when necessary) or too crowded for patients that might experience neutropenia, using POCT instruments could be a more efficient alternative for both the patient and the physician.
Finally, POCT troponin could be an option for screening of cardiovascular risk in the general and high-risk populations. Multiple papers have demonstrated that troponins are excellent predictors of long-term risks of adverse cardiovascular events and mortality (23-27). These studies indicate that hs-cTnI may be the best predictor of future myocardial infarction whilst hs-cTnT may be better for predicting all-cause mortality. However, troponin screening or monitoring is not yet recommended, as there are few possible interventions after the increased risk is established, and currently no consensus on preventive treatment exists. If evidence shows that troponin guided interventions may reduce long-term cardiovascular risk, primary care physician and out-patient clinics accustomed to using POCT in monitoring chronic conditions (e.g., diabetes monitoring is already done by POCT in some regions) might want to use POCT instruments for screening or monitoring purposes. Rapid results would be particularly useful if troponin-guided interventions were to be implemented. The primary care physician would then have an opportunity for adjusting treatment without the delay (and increased work) from laboratory results being available hours or days after the patient visit.
Use of hs-cTn POCT as back-up instruments
Smaller hospitals or health care facilities that provide acute care usually include a central laboratory platform for providing laboratory analysis. Such facilities might be able to process the daily sample volume by using one central laboratory instrument/module. However, two instruments/modules will typically be in place to provide backup facilities. In such laboratories, a POCT instrument could be an attractive and cost-effective possibility as a backup instrument, especially if this instrument is able to process other biomarkers typically requested in acute situations (like D-dimer, CRP, NT-proBNP). Another scenario is when trained laboratory staff are not available on a 24/7 basis. This might be routine in rural acute health care facilities, especially during the night shift when the number of requests are low. In these cases, a POCT instrument operated by non-laboratory staff could provide access to hs-cTn results, without the need for 24-hour laboratory cover. It should be noted that such or similar approach must take the lack of standardization between hs-cTn assays into account; workup in individual patients should be done with the same assay and assays-specific cut-offs must be implemented as applicable.
What scientific data do we need before novel troponin (POCT) assays may be implemented in daily practice?
In principle, the same basic data is required for all hs-cTn assays (CLT and POCT) before implementation in routine practice (52). On the laboratory side this refers to the assay characteristics determined in accordance with the applicable guidelines from Clinical and Laboratory Standards Institute, as listed in the tables provided by the IFCC C-CB (29) which includes limits of blank, detection and quantification, analytical variation, sex specific 99th percentile upper reference limits, reportable range, accuracy, proportion measurable results in healthy individuals and interfering substances. For POCT instrument data demonstrating practicality and user friendliness should also be provided. These evaluations should preferably be undertaken independently from the manufacturer as applicability is, in general, higher. In the U.S., testing is given waived-, moderate- or high-complexity testing status that dictates the qualifications for use. To increase the availability of POCT assays in areas without qualified lab technologist in the U.S, test complexities need to be assigned to available POCT assays. On the clinical side, diagnostic performance for AMI, accuracy (sensitivity, specificity, predictive values and area under receiver operating curves) and efficiency for early rule-in and rule-out of patients with and without NSTEMI using different baseline cut-offs and/or delta values should be documented, for all relevant matrixes. Cut-offs and/or delta values represents a challenge as the need for whole blood makes biobanked sample material available from earlier well-described observational studies inapplicable for validating a new POCT device. Furthermore, in the early implementation phase real life data describing long-term analytical performance (lot to lot variations) should be reported, since safety and efficiency of clinical cut-offs are highly dependent on assay stability. Earlier studies shows that even a slight bias (shift) have the potential to largely impact the number of ruled-out patients and performance of algorithms (53-55).
Laboratory costs related to POCT assays are usually higher compared to CLT, and use of POCT assays are therefore generally only indicated when this technology improves clinical care compared to CLT. The benefits should be clearly described and documented before the POCT assay is implemented. As the reduced TAT for POCT assays might not automatically be translated into reduced length of stay in the ED or elsewhere the expected effects of implementing POCT should be scientifically tested, preferable through randomized controlled trials (56). Safety, efficiency and cost-effectivity of prehospital hs-cTn POCT should also be investigated as this might have a potential for considerable reduction in patient influx to EDs and hospitals.
Institutional preparations before implementing POCT
There are numerous practical issues that need to be in place before a POCT instrument may be implemented in an institution. Some matters are relatively easily solved such as need for a physical space with power supply and online connection for the device. Storage-room for the cartridges close to the site of analysis might have specific temperature requirements (refrigeration) for some assays. Integration with the laboratory information system should be in place, ensuring direct transmission into the patient files, increasing patient safety. Standard laboratory quality assessment schemes like internal (IQA) and external (EQA) quality assessment should be implemented. The frequency of IQA for POCT instruments are usually lower compared to CLT, and once weekly or even monthly may be used, depending on national practice or legal requirements, recommendations from the manufacturers and in-house experience with the instrument. The lower frequency of IQA might have a positive impact on cost-effectiveness, however performing IQA in the ED may be more labour intensive for the laboratory staff and the use of in-house produced IQA material may be less feasible. EQA schemes for contemporary POCT cTn assays are available and may be used by hs-cTn assays, although EQA providers should adjust the concentrations of EQA samples to reflect the diagnostic cut-offs applicable for high-sensitivity assays. Regular inter-instrument comparison using whole blood to monitor the difference between the instruments could be useful, especially if small delta values are utilized as clinical cut-offs, in rule-out and rule-in algorithms. Finally, the staff who should use the device needs proper training. This may be a time-consuming effort in larger EDs with high number of employees working in around the clock shifts. Quality assurance, instrument maintenance and training might preferably be centralized to increase expertise. Point-of-care coordinators (POCC) have already been established in some regions and could play a pivotal role in management of POCT. POCC could have an especially important role maintaining the obligatory quality assurance and hygiene requirements (including an effective and complete decontamination of the devices) that musts be implemented in EDs and less traditional settings, such as prehospital services or nursing homes.
It is crucial to acknowledge that skilled personnel, both in clinical and laboratory settings, is a limited resource and POCT may be associated with an additional workload for non-laboratory staff. POCT generally involves a direct transfer of blood sampling and biochemical analyses form laboratory personnel directly to caregivers. Changes in staff or workflow within the department will typically be necessary. Thus, conducting a thorough evaluation of the local context is necessary before implementing POCT. Factors such as current work-load and recruitment status of the staff involved should be weighed against potential benefits.
Realising the efficiency benefits of POCT in an institution is dependent on the clinical staffs’ adherence to and trust in the new and more rapid approach. To achieve this, several measures should be taken. There should be a clear written guidance within the institution for when a hs-cTn POCT sample is indicated and how the results should be interpreted. If the institution intends to use two different hs-cTn assays (POCT in the ED and CLT in remaining departments) a well-defined routine for managing the transition from POCT to CLT should be established. This should acknowledge the low concordance between hs-cTn assays requiring assay specific cut-offs, so that a regime for retesting initial samples with CLT or further testing for patients admitted might be necessary. The recommendations should be audited, endorsed and well known to all relevant stakeholders before implementation. This will include the ED physicians, care pathway staff, nurses, cardiologists and laboratory staff. Usually, the guidance should be based on national or international guidelines to reassure all staff and clinicians of all experience levels of their validity.
Furthermore, several multicentre studies have documented that the impact of POCT is dependent on the local settings and logistics where it is used (42,57). Accordingly, there might be a need for organizational changes to support POCT and more rapid algorithms. This may encompass re-organizing the ED or establishing outpatient clinics that undertake follow-up of patients ruled-out for NSTEMI who need investigations for other conditions.
Conclusions
Hs-cTn POCT assays have become available and are expected to lead to increased efficiency and improved clinical decision making for patients in a broad range of clinical setting. In most clinical scenarios POCT cTn assays need similar analytical and clinical performance as central laboratory hs-cTn assays. Utility of POCT also requires scientific data demonstrating user-friendliness, increased efficiency and improved cost-effectivity compared to CLT. Large numbers of educational and practical measures are necessary before a new routine involving POCT may be established. Future studies are needed to provide the necessary data and further investigate the benefits and utilities of hs-cTn POCT assays.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Xander van Wijk, Amy Saenger, Steven Meex, and Allan Jaffe) for the series “Cardiac Troponin” published in Journal of Laboratory and Precision Medicine. The article has undergone external peer review.
Peer Review File: Available at https://jlpm.amegroups.com/article/view/10.21037/jlpm-23-3/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jlpm.amegroups.com/article/view/10.21037/jlpm-23-3/coif). The series “Cardiac Troponin” was commissioned by the editorial office without any funding or sponsorship. KMA is an associate editor of Clinical Biochemistry and chair of the IFCC Committee on Clinical Applications of Cardiac Bio-Markers (C-CB), she has served on the advisory board for Roche Diagnostics and SpinChip, received consultant honoraria from CardiNor, lecturing honorarium from Siemens Healthineers and Snibe Diagnostics and research grants from Siemens Healthineers and Roche Diagnostics. PC is an associate editor of the Journal of Applied Laboratory Medicine and on the advisory board of Psyros Diagnostics and Radiometer and has previously advised and Siemens. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cummins B, Auckland ML, Cummins P. Cardiac-specific troponin-I radioimmunoassay in the diagnosis of acute myocardial infarction. Am Heart J 1987;113:1333-44. [Crossref] [PubMed]
- Katus HA, Remppis A, Looser S, et al. Enzyme linked immuno assay of cardiac troponin T for the detection of acute myocardial infarction in patients. J Mol Cell Cardiol 1989;21:1349-53. [Crossref] [PubMed]
- Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal Definition of Myocardial Infarction (2018). Circulation 2018;138:e618-51. [Crossref] [PubMed]
- Apple FS, Jesse RL, Newby LK, et al. National Academy of Clinical Biochemistry and IFCC Committee for Standardization of Markers of Cardiac Damage Laboratory Medicine Practice Guidelines: Analytical issues for biochemical markers of acute coronary syndromes. Circulation 2007;115:e352-5. [Crossref] [PubMed]
- Wu AHB, Christenson RH, Greene DN, et al. Clinical Laboratory Practice Recommendations for the Use of Cardiac Troponin in Acute Coronary Syndrome: Expert Opinion from the Academy of the American Association for Clinical Chemistry and the Task Force on Clinical Applications of Cardiac Bio-Markers of the International Federation of Clinical Chemistry and Laboratory Medicine. Clin Chem 2018;64:645-55. [Crossref] [PubMed]
- Sandoval Y, Apple FS, Saenger AK, et al. 99th Percentile Upper-Reference Limit of Cardiac Troponin and the Diagnosis of Acute Myocardial Infarction. Clin Chem 2020;66:1167-80. [Crossref] [PubMed]
- Apple FS. A new season for cardiac troponin assays: it's time to keep a scorecard. Clin Chem 2009;55:1303-6. [Crossref] [PubMed]
- Aakre KM, Saenger AK, Body R, et al. Analytical Considerations in Deriving 99th Percentile Upper Reference Limits for High-Sensitivity Cardiac Troponin Assays: Educational Recommendations from the IFCC Committee on Clinical Application of Cardiac Bio-Markers. Clin Chem 2022;68:1022-30. [Crossref] [PubMed]
- Reichlin T, Hochholzer W, Bassetti S, et al. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med 2009;361:858-67. [Crossref] [PubMed]
- Keller T, Zeller T, Peetz D, et al. Sensitive troponin I assay in early diagnosis of acute myocardial infarction. N Engl J Med 2009;361:868-77. [Crossref] [PubMed]
- Neumann JT, Twerenbold R, Ojeda F, et al. Application of High-Sensitivity Troponin in Suspected Myocardial Infarction. N Engl J Med 2019;380:2529-40. [Crossref] [PubMed]
- Anand A, Lee KK, Chapman AR, et al. High-Sensitivity Cardiac Troponin on Presentation to Rule Out Myocardial Infarction: A Stepped-Wedge Cluster Randomized Controlled Trial. Circulation 2021;143:2214-24. [Crossref] [PubMed]
- Chapman AR, Anand A, Boeddinghaus J, et al. Comparison of the Efficacy and Safety of Early Rule-Out Pathways for Acute Myocardial Infarction. Circulation 2017;135:1586-96. [Crossref] [PubMed]
- Shah ASV, Anand A, Strachan FE, et al. High-sensitivity troponin in the evaluation of patients with suspected acute coronary syndrome: a stepped-wedge, cluster-randomised controlled trial. Lancet 2018;392:919-28. [Crossref] [PubMed]
- Wildi K, Boeddinghaus J, Nestelberger T, et al. Comparison of fourteen rule-out strategies for acute myocardial infarction. Int J Cardiol 2019;283:41-7. [Crossref] [PubMed]
- Lopez-Ayala P, Boeddinghaus J, Koechlin L, et al. Early Rule-Out Strategies in the Emergency Department Utilizing High-Sensitivity Cardiac Troponin Assays. Clin Chem 2021;67:114-23. [Crossref] [PubMed]
- Twerenbold R, Neumann JT, Sörensen NA, et al. Prospective Validation of the 0/1-h Algorithm for Early Diagnosis of Myocardial Infarction. J Am Coll Cardiol 2018;72:620-32. [Crossref] [PubMed]
- Westwood M, Ramaekers B, Grimm S, et al. High-sensitivity troponin assays for early rule-out of acute myocardial infarction in people with acute chest pain: a systematic review and economic evaluation. Health Technol Assess 2021;25:1-276. [Crossref] [PubMed]
- Chew DP, Lambrakis K, Blyth A, et al. A Randomized Trial of a 1-Hour Troponin T Protocol in Suspected Acute Coronary Syndromes: The Rapid Assessment of Possible Acute Coronary Syndrome in the Emergency Department With High-Sensitivity Troponin T Study (RAPID-TnT). Circulation 2019;140:1543-56. [Crossref] [PubMed]
- Collet JP, Thiele H, Barbato E, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 2021;42:1289-367. [Crossref] [PubMed]
- Halvorsen S, Mehilli J, Cassese S, et al. 2022 ESC Guidelines on cardiovascular assessment and management of patients undergoing non-cardiac surgery. Eur Heart J 2022;43:3826-924. [Crossref] [PubMed]
- Lyon AR, López-Fernández T, Couch LS, et al. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS). Eur Heart J 2022;43:4229-361. [Crossref] [PubMed]
- Omland T, de Lemos JA, Sabatine MS, et al. A sensitive cardiac troponin T assay in stable coronary artery disease. N Engl J Med 2009;361:2538-47. [Crossref] [PubMed]
- de Lemos JA, Drazner MH, Omland T, et al. Association of troponin T detected with a highly sensitive assay and cardiac structure and mortality risk in the general population. JAMA 2010;304:2503-12. [Crossref] [PubMed]
- Seliger SL, Hong SN, Christenson RH, et al. High-Sensitive Cardiac Troponin T as an Early Biochemical Signature for Clinical and Subclinical Heart Failure: MESA (Multi-Ethnic Study of Atherosclerosis). Circulation 2017;135:1494-505. [Crossref] [PubMed]
- Lyngbakken MN, Røsjø H, Holmen OL, et al. Gender, High-Sensitivity Troponin I, and the Risk of Cardiovascular Events (from the Nord-Trøndelag Health Study). Am J Cardiol. 2016;118:816-21. [Crossref] [PubMed]
- Parikh RH, Seliger SL, de Lemos J, et al. Prognostic Significance of High-Sensitivity Cardiac Troponin T Concentrations between the Limit of Blank and Limit of Detection in Community-Dwelling Adults: A Metaanalysis. Clin Chem 2015;61:1524-31. [Crossref] [PubMed]
- Collinson P, Aakre KM, Saenger A, et al. Cardiac troponin measurement at the point of care: educational recommendations on analytical and clinical aspects by the IFCC Committee on Clinical Applications of Cardiac Bio-Markers (IFCC C-CB). Clin Chem Lab Med 2023;61:989-98. [Crossref] [PubMed]
- High-Sensitivity* Cardiac Troponin I and T Assay Analytical Characteristics Designated by Manufacturer. IFCC Committee on Clinical Applications of Cardiac Bio-Markers (C-CB) v052022. Available online: https://ifcc.org/ifcc-education-division/emd-committees/committee-on-clinical-applications-of-cardiac-bio-markers-c-cb/biomarkers-reference-tables/
- Sun BC, Hsia RY, Weiss RE, et al. Effect of emergency department crowding on outcomes of admitted patients. Ann Emerg Med 2013;61:605-11.e6. [Crossref] [PubMed]
- Jones S, Moulton C, Swift S, et al. Association between delays to patient admission from the emergency department and all-cause 30-day mortality. Emerg Med J 2022;39:168-73. [Crossref] [PubMed]
- Apple FS, Smith SW, Greenslade JH, et al. Single High-Sensitivity Point-of-Care Whole-Blood Cardiac Troponin I Measurement to Rule Out Acute Myocardial Infarction at Low Risk. Circulation 2022;146:1918-29. [Crossref] [PubMed]
- Sandoval Y, Lewis BR, Mehta RA, et al. Rapid Exclusion of Acute Myocardial Injury and Infarction With a Single High-Sensitivity Cardiac Troponin T in the Emergency Department: A Multicenter United States Evaluation. Circulation 2022;145:1708-19. [Crossref] [PubMed]
- Steiro OT, Tjora HL, Langørgen J, et al. Clinical risk scores identify more patients at risk for cardiovascular events within 30 days as compared to standard ACS risk criteria: the WESTCOR study. Eur Heart J Acute Cardiovasc Care 2021;10:287-301. [Crossref] [PubMed]
- Collinson P, Hammerer-Lercher A, Suvisaari J, et al. How Well Do Laboratories Adhere to Recommended Clinical Guidelines for the Management of Myocardial Infarction: The CARdiac MArker Guidelines Uptake in Europe Study (CARMAGUE). Clin Chem 2016;62:1264-71. [Crossref] [PubMed]
- Nowak RM, Jacobsen G, Limkakeng A Jr, et al. Outpatient versus observation/inpatient management of emergency department patients rapidly ruled-out for acute myocardial infarction: Findings from the HIGH-US study. Am Heart J 2021;231:6-17. [Crossref] [PubMed]
- Sanders JH, Karr T. Improving ED specimen TAT using Lean Six Sigma. Int J Health Care Qual Assur 2015;28:428-40. [Crossref] [PubMed]
- Collinson PO, John C, Lynch S, et al. A prospective randomized controlled trial of point-of-care testing on the coronary care unit. Ann Clin Biochem 2004;41:397-404. [Crossref] [PubMed]
- Goodacre SW, Bradburn M, Cross E, et al. The Randomised Assessment of Treatment using Panel Assay of Cardiac Markers (RATPAC) trial: a randomised controlled trial of point-of-care cardiac markers in the emergency department. Heart 2011;97:190-6. [Crossref] [PubMed]
- Loten C, Attia J, Hullick C, et al. Point of care troponin decreases time in the emergency department for patients with possible acute coronary syndrome: a randomised controlled trial. Emerg Med J 2010;27:194-8. [Crossref] [PubMed]
- Renaud B, Maison P, Ngako A, et al. Impact of point-of-care testing in the emergency department evaluation and treatment of patients with suspected acute coronary syndromes. Acad Emerg Med 2008;15:216-24. [Crossref] [PubMed]
- Ryan RJ, Lindsell CJ, Hollander JE, et al. A multicenter randomized controlled trial comparing central laboratory and point-of-care cardiac marker testing strategies: the Disposition Impacted by Serial Point of Care Markers in Acute Coronary Syndromes (DISPO-ACS) trial. Ann Emerg Med 2009;53:321-8. [Crossref] [PubMed]
- Boeddinghaus J, Nestelberger T, Koechlin L, et al. Early Diagnosis of Myocardial Infarction With Point-of-Care High-Sensitivity Cardiac Troponin I. J Am Coll Cardiol 2020;75:1111-24. [Crossref] [PubMed]
- Sörensen NA, Neumann JT, Ojeda F, et al. Diagnostic Evaluation of a High-Sensitivity Troponin I Point-of-Care Assay. Clin Chem 2019;65:1592-601. [Crossref] [PubMed]
- Harskamp RE, Laeven SC, Himmelreich JC, et al. Chest pain in general practice: a systematic review of prediction rules. BMJ Open 2019;9:e027081. [Crossref] [PubMed]
- Goodacre S, Cross E, Arnold J, et al. The health care burden of acute chest pain. Heart 2005;91:229-30. [Crossref] [PubMed]
- Langlo NM, Orvik AB, Dale J, et al. The acute sick and injured patients: an overview of the emergency department patient population at a Norwegian University Hospital Emergency Department. Eur J Emerg Med 2014;21:175-80. [Crossref] [PubMed]
- Tolsma RT, Fokkert MJ, van Dongen DN, et al. Referral decisions based on a pre-hospital HEART score in suspected non-ST-elevation acute coronary syndrome: final results of the FamouS Triage study. Eur Heart J Acute Cardiovasc Care 2022;11:160-9. [Crossref] [PubMed]
- Johannessen TR, Vallersnes OM, Halvorsen S, et al. Pre-hospital One-Hour Troponin in a Low-Prevalence Population of Acute Coronary Syndrome: OUT-ACS study. Open Heart 2020;7:e001296. [Crossref] [PubMed]
- Johannessen TR, Halvorsen S, Atar D, et al. Cost-effectiveness of a rule-out algorithm of acute myocardial infarction in low-risk patients: emergency primary care versus hospital setting. BMC Health Serv Res 2022;22:1274. [Crossref] [PubMed]
- Koper LH, Frenk LDS, Meeder JG, et al. URGENT 1.5: diagnostic accuracy of the modified HEART score, with fingerstick point-of-care troponin testing, in ruling out acute coronary syndrome. Neth Heart J 2022;30:360-9. [Crossref] [PubMed]
- Christenson RH, Frenk LDS, de Graaf HJ, et al. Point-of-Care: Roadmap for Analytical Characterization and Validation of a High-Sensitivity Cardiac Troponin I Assay in Plasma and Whole Blood Matrices. J Appl Lab Med 2022;7:971-88. [Crossref] [PubMed]
- Haagensen K, Collinson P, Åsberg A, et al. How Does the Analytical Quality of the High-Sensitivity Cardiac Troponin T Assay Affect the ESC Rule Out Algorithm for NSTEMI? Clin Chem 2019;65:494-6. [Crossref] [PubMed]
- Tjora HL, Steiro OT, Langørgen J, et al. Cardiac Troponin Assays With Improved Analytical Quality: A Trade-Off Between Enhanced Diagnostic Performance and Reduced Long-Term Prognostic Value. J Am Heart Assoc 2020;9:e017465. [Crossref] [PubMed]
- Tjora HL, Steiro OT, Langørgen J, et al. Diagnostic Performance of Novel Troponin Algorithms for the Rule-Out of Non-ST-Elevation Acute Coronary Syndrome. Clin Chem 2022;68:291-302. [Crossref] [PubMed]
- Price CP, Christenson RH. Evidence based Laboratory Medicine; Principles, Practice, and Outcomes. 2nd ed. Washington, DC: AACC Press; 2007.
- Bradburn M, Goodacre SW, Fitzgerald P, et al. Interhospital variation in the RATPAC trial (Randomised Assessment of Treatment using Panel Assay of Cardiac markers). Emerg Med J 2012;29:233-8. [Crossref] [PubMed]
Cite this article as: Thulin IVL, Myrmel GMS, Jordalen SMF, Collinson P, Aakre KM. Point-of-care high-sensitivity troponin assays: advancements, clinical applications, and implementation considerations. J Lab Precis Med 2023;8:20.


