
Vitamin D status during the COVID-19 pandemic: a pragmatic approach to measurement and supplementation
In a recent article published in this journal, Bretz and colleagues (1) report the interesting results of a vitamin D [25-hydroxyvitamin D (25OH-D)] investigation conducted in Brazilian patients in two different epochs, i.e., in the pre-pandemic (years 2018–2019) and pandemic (years 2020–2021) periods of coronavirus disease 2019 (COVID-19). Overall, the 25OH-D levels were found slightly but significantly decreased during the pandemic compared to the pre-pandemic period (−10%; 26.9 vs. 29.6 ng/mL; P<0.001). This is a relatively unexpected finding, as there is controversial evidence on this topic. Kwon et al. screened 1,483 Korean adults aged ≥19 years (2), and reported that the mean 25OH-D levels increased significantly during the national COVID-19 lockdown compared with the pre-pandemic period (23.6 vs. 21.4 ng/mL; P<0.001). In another study, we measured serum levels of 25OH-D in Italian subjects aged ≥18 years (3), and found that the hormone concentration did not significantly differ during the national COVID-19 lockdown compared to the same period of the previous two years (31.2 vs. 30.8 ng/mL; P=0.277). Consistent with these findings, Meoli et al. conducted a cross-sectional study in which serum 25OH-D levels were measured in 298 Swiss adolescents aged 18–19 years between July and December 2020 (4), and were compared with values obtained in a cohort of 437 matched adolescents from the years 2014–2016. During the pandemic, the serum levels of 25OH-D did not differ from the pre-pandemic period (30.8 vs. 29.6 ng/mL; P=0.50).
So where does the truth lie? Did the COVID-19 pandemic really contribute to lower serum 25OH-D levels in certain populations, or is the relatively short duration of social restrictions (including lockdown and home confinement of positive cases) failing to generate a substantial impact on 25OH-D status? There is no simple answer to this question. The likelihood of developing 25OH-D deficiency depends on a kaleidoscope of demographic (age, sex, ethnicity, skin phenotype), clinical (renal function, malabsorption, therapies), lifestyle (diet, physical activity), and environmental conditions (sun exposure, seasonality) (5). No study designs or populations are therefore directly comparable to others, and this may largely help to explain why different investigations may yield even opposite findings.
A second important consideration that needs to be made is the impact of 25OH-D deficiency on human health and, in particular, on COVID-19. A recent meta-analysis that included 21 studies showed that mortality did not differ significantly between COVID-19 patients with deficient and sufficient 25OH-D levels [relative risk (RR), 1.60; 95% confidence interval (CI): 0.93–2.27] (6). Moreover, the results of a recent systematic literature review and meta-analysis of randomized controlled trials showed that 25OH-D supplementation did not contribute to improve the clinical course of COVID-19 (7), since it did not improve the risk of death (RR, 0.94; 95% CI: 0.69–1.29; P=0.7), intensive care unit (ICU) admission (RR, 0.64; 95% CI: 0.38–1.08; P=0.1), and mechanical ventilation or intubation (RR, 0.77; 95% CI: 0.58–1.02; P=0.1). Similar evidence emerged from another meta-analysis by Sîrbu and colleagues (8), published almost simultaneously, in which mortality in COVID-19 patients did not differ between those who did or did not receive 25OH-D supplementation (RR, 0.93; 95% CI: 0.57–1.52; P=0.78), although a marginally significant effect was found in terms of reduction in ICU admission (RR, 0.63; 95% CI: 0.41–0.99; P=0.04).
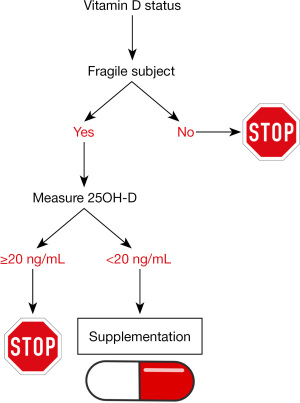
Overall, the situation is hence quite controversial, confirming previous evidence that public health policies based on 25OH-D supplementation (including food fortification) have uncertain effects on reducing the risk of adverse outcomes of acute or chronic diseases in the general population (9). It seems more appropriate to assert that the beneficial effects of 25OH-D supplementation may be limited to individuals with overt deficiency (e.g., <20 ng/mL) (10), who could benefit most from correcting their deficit. In summary, a pragmatic approach might be to routinely determine 25OH-D status in the most vulnerable and susceptible groups of the general population (i.e., patients with advanced age, multiple comorbidities, immunosuppression) who are at higher risk for developing adverse outcomes of COVID-19 and other severe of life-threatening pathologies, and to reserve vitamin D supplementation to those who are clearly deficient, as summarized in Figure 1.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was a standard submission to the journal. The article did not undergo external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://jlpm.amegroups.org/article/view/10.21037/jlpm-23-73/coif). G.L. serves as the Editor-in-Chief of Journal of Laboratory and Precision Medicine. The other author has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bretz GPM, Campos JR, Veloso AA, et al. Impact of COVID-19 pandemic on serum 25-hydroxyvitamin D levels in Brazilian patients. J Lab Precis Med 2023;8:31. [Crossref]
- Kwon JY, Kang SG. Changes in Vitamin D Status in Korean Adults during the COVID-19 Pandemic. Nutrients 2022;14:4863. [Crossref] [PubMed]
- Lippi G, Ferrari A, Targher G. Is COVID-19 lockdown associated with vitamin D deficiency? Eur J Public Health 2021;31:278-9. [Crossref] [PubMed]
- Meoli M, Muggli F, Lava SAG, et al. Vitamin D Status in Adolescents during COVID-19 Pandemic: A Cross-Sectional Comparative Study. Nutrients 2021;13:1467. [Crossref] [PubMed]
- Lippi G, Mattiuzzi C, Aloe R. The impact of seasonality and other determinants on vitamin D concentration in childhood and adulthood: still an unresolved issue. Ann Transl Med 2016;4:21. [PubMed]
- Bignardi PR, de Andrade Castello P, de Matos Aquino B, et al. Is the vitamin D status of patients with COVID-19 associated with reduced mortality? A systematic review and meta-analysis. Arch Endocrinol Metab 2023;67:276-88. [Crossref] [PubMed]
- Zhang Y, Li J, Yang M, et al. Effect of vitamin D supplementation on COVID-19 patients: A systematic review and meta-analysis. Front Nutr 2023;10:1131103. [Crossref] [PubMed]
- Sîrbu AC, Sabin O, Bocșan IC, et al. The Effect of Vitamin D Supplementation on the Length of Hospitalisation, Intensive Care Unit Admission, and Mortality in COVID-19-A Systematic Review and Meta-Analysis. Nutrients 2023;15:3470. [Crossref] [PubMed]
- Lippi G, Targher G. Are we overrating the extra-skeletal benefits of oral vitamin D supplementation? Ann Transl Med 2019;7:499. [Crossref] [PubMed]
- Hossein-nezhad A, Holick MF. Vitamin D for health: a global perspective. Mayo Clin Proc 2013;88:720-55. [Crossref] [PubMed]
Cite this article as: Lippi G, Mattiuzzi C. Vitamin D status during the COVID-19 pandemic: a pragmatic approach to measurement and supplementation. J Lab Precis Med 2024;9:10.


